
Participants sharing a moment together at the iconic Ivory Tower, Makerere University
From June 23 to 27, 2025, the Polygenic Risk Score (PRS) Analysis Course 2025 convened at the Infectious Diseases Institute (IDI) of Makerere University in Kampala, Uganda. Organized by the African Center of Excellence in Bioinformatics and Data Intensive Sciences (ACE-Uganda), this intensive five-day program gathered over 40 early-career scientists, geneticists, and bioinformaticians from Uganda, Kenya, Tanzania, Rwanda, and beyond. Drawing inspiration from global initiatives like Wellcome Connecting Science’s PRS courses for Africa, the event targeted researchers in bioinformatics, genetic epidemiology, population genetics, and statistical genetics, emphasizing practical skills for diverse populations.
For newcomers to genomics, polygenic risk scores offer a powerful lens on complex diseases. Unlike single-gene disorders, traits like type 2 diabetes, hypertension, or schizophrenia arise from thousands of common genetic variants, each contributing small effects. A PRS aggregates these—typically single nucleotide polymorphisms (SNPs)—into a single metric: a weighted sum where each variant’s score reflects its effect size from genome-wide association studies (GWAS). The formula is straightforward: PRS = Σ (β_i × G_i), where β_i is the effect size of SNP i, and G_i is the genotype dosage (0, 1, or 2 risk alleles). This yields a normally distributed score across populations, with higher values signaling elevated risk. In Europeans, PRS can explain 10-20% of variance for traits like height or coronary artery disease, aiding risk stratification. Yet, global utility hinges on addressing biases: over 90% of GWAS data is European-derived, inflating scores for that ancestry while underperforming elsewhere due to linkage disequilibrium (LD) differences and allele frequency shifts.
The PRS Portability Problem loomed large in the curriculum, a critical barrier for African applications. Portability refers to how well a PRS trained on one ancestry predicts in another—often dropping 30-60% in accuracy for Africans, driven by greater genetic diversity and rarer causal alleles in European data. Participants dissected this through lectures on ancestry-specific GWAS, LD patterns, and allele frequency divergences. Real-world stakes? In Africa, where non-communicable diseases like hypertension affect 30% of adults and infectious threats like HIV persist, tailored PRS could personalize screening or therapies—but only if portable.
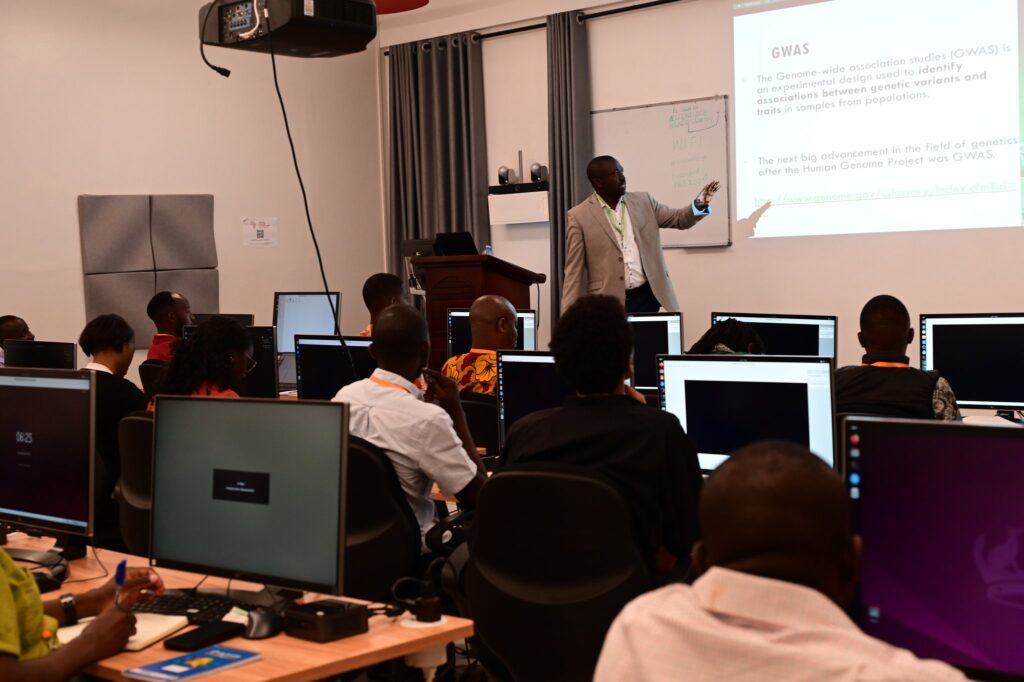
Professor Segun Fatumo sharing about GWAs at the Polygenic Risk Score (PRS) Analysis Course, Day One
Day one grounded theory: GWAS fundamentals, heritability estimation via tools like LD Score Regression, and PRS construction pipelines. Experts from ACE-Uganda and international collaborators introduced the Clumping + Thresholding (C+T) method—pruning SNPs in LD (r² < 0.1 within 250kb) then selecting by p-value thresholds (e.g., 5×10⁻⁸ to 0.5)—alongside advanced Bayesian approaches like PRS-CS or LDpred for posterior effect size shrinkage. Hands-on sessions used Google Colab for cloud access, bypassing hardware barriers.
Core practicals spanned days two to four, leveraging open-source tools. Attendees imported GWAS summary statistics via R’s data.table, quality-controlled with PLINK 2.0 (filtering MAF >0.01, INFO >0.8), and computed PRS using PRSice-2—a C++-powered software integrating PLINK for efficiency. For a hypertension example, groups processed European GWAS data (e.g., from UK Biobank) on African target genotypes, visualizing scores in R with ggplot2. Key lesson: Evaluate via R² (variance explained) or AUC for binary traits, adjusting for principal components to mitigate population stratification.
A spotlight was PRS adaptation for diversity. Participants applied BridgePRS, a Bayesian method borrowing shared effects across ancestries to boost portability—yielding 61% higher R² in African simulations. They tackled admixed samples, estimating local ancestry with RFMix to weight scores, addressing the “mosaic” genomes common in African diaspora. Group projects modeled real African datasets: one team refined a type 2 diabetes PRS using H3Africa summary stats, revealing ancestry-enriched variants near SLC16A11 for improved prediction; another explored schizophrenia portability, integrating multi-ancestry meta-GWAS to counter Euro-bias. Limitations surfaced too—PRS explain <10% variance in Africans for most traits, demanding integration with clinical or environmental factors.
We extend deep gratitude to supporters like Wellcome Connecting Science and Google DeepMind, whose funding and expertise enabled scholarships for 70% of attendees, cloud compute credits, and guest seminars on equitable genomics. Their BioStruct-Africa-like initiatives have trained 300+ African scientists since 2023, providing open resources like the PGS Catalog for downloading pre-computed scores. This partnership, aligned with NIAID consortia, underscores a push for inclusive data: by 2025, African-inclusive GWAS have doubled PRS accuracy for hemoglobin traits, vital for sickle cell research.
Networking wove through: 1:1 mentorship, alumni panels on PRS in Ebola susceptibility studies, and cross-border brainstorming for Rift Valley fever genomics. Surveys showed 92% of participants ready to deploy PRS in labs, with plans for peer training.
For bioinformatics seekers, this course models accessible ramps. Start with PRSice-2 tutorials or the Nature Protocols guide for end-to-end workflows. Beginners: Download sample data from 1000 Genomes, compute a height PRS, and plot quantile risks. Pro tip: Always validate cross-ancestry with metrics like Nagelkerke’s R², and explore multi-omic boosts like transcriptome risk scores for 20% portability gains in Africans.
ACE-Uganda’s drive for African-led innovation shines here. As PRS evolve—with tools like PolyPred fine-mapping functional variants—envision local therapies for cardiometabolic burdens or HIV progression. This course didn’t just impart skills; it seeded equitable genomic futures. Join us—Africa’s data revolution awaits.
